By Joshua Schneyer and M.B. Pell/Reuters
LEETONIA, Ohio – When Jennifer Sekerak took son Joshua for his age-one check-up, the pediatrician saw no need to test for lead poisoning. The baby wasn’t yet walking, she recalls the doctor saying, so was unlikely to be playing around hazards like lead paint.
Over the next year or so, Joshua was twice hospitalized for mysterious symptoms. He began refusing food and eating dirt. There was violent head-banging, sleeplessness, skin lesions, vomiting.
“He stopped talking, he wanted to eat dirt, and he would scream like a banshee,” Sekerak said. “To be honest, he was like a wild animal.”
Once, Joshua was rushed to the hospital in Boardman, Ohio, and diagnosed with severe anemia, a common finding in lead-poisoned children. Hospital staff told Sekerak her son, enrolled in Medicaid, might have lead poisoning. But the hospital, Akron Children’s at Boardman, did not test his blood for lead, she says. Citing federal privacy rules, a hospital spokeswoman declined comment.
At the mother’s urging, a new pediatrician tested him at age two. His blood lead concentration was 19 micrograms per deciliter, nearly four times the level Ohio defines as lead poisoning and the Centers for Disease Control and Prevention considers elevated. Had Joshua been tested earlier – as Medicaid and Ohio rules required – the family could have more quickly removed him from a lead-infested rental house, Sekerak said.
Joshua’s case is not unique, a Reuters investigation found. Nationwide, millions of children are falling through the cracks of early childhood lead testing requirements.
 (ENLARGE)
(ENLARGE)
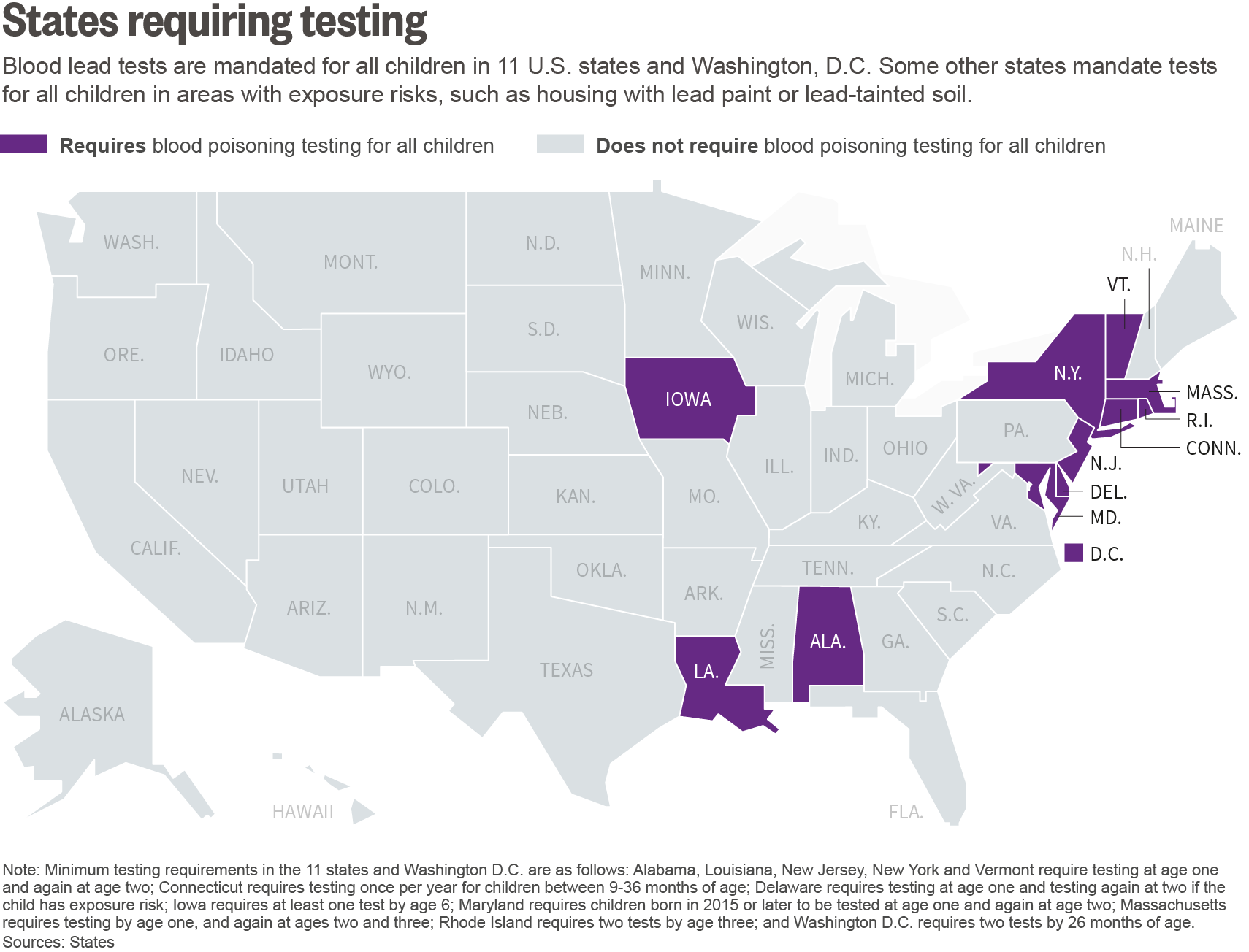
Blood lead tests are mandated for all children in 11 U.S. states and Washington, DC. In addition, Medicaid requires that the one-third of all U.S. children enrolled in the program, which provides health care for low-income and disabled people, be tested at ages one and two. Some other states mandate tests for all children in areas with exposure risks, such as housing with lead paint or lead-tainted soil.
Yet, in a review of data in nearly a dozen U.S. states, Reuters found just 41 percent of Medicaid-enrolled one- and two-year-olds had been tested as required. And in some states requiring tests, more than half the children were missing a test.
The full scope of under-testing is impossible to gauge: Data tracking testing rates and results from the CDC, Medicaid and many state health agencies is incomplete and unreliable. The CDC said its own tracking of lead poisoning rates isn’t conclusive, citing insufficient data from states and changes in testing patterns that make comparisons over time challenging.
Yet Reuters documented a sweeping testing gap in the data that could be verified.
The shortfalls leave some children vulnerable to prolonged lead exposure, among the most insidious, and preventable, early health risks. Lead poisoning can lead to a lifetime of severe mental and physical ailments.
Some 500,000 U.S. children under age six have blood lead levels of 5 micrograms per deciliter or higher, the CDC estimates, the level at which it suggests “public health actions.”
“When we fail to provide lead poisoning tests to children who need them, it’s a tragedy,” said Dr. Leonardo Trasande, associate professor of pediatrics at New York University School of Medicine. “Unfortunately, a lot of pediatricians and health care providers have taken their eye off this ball.”
Concerns about lead exposure grew dramatically after news that the water supply in Flint, Michigan had been poisoned.
Michigan does not require universal testing for lead exposure, and state officials only began to acknowledge a serious water contamination problem in Flint months after a local pediatrician showed them evidence: Lead levels in her patients’ blood were spiking over the CDC’s threshold.
“If you don’t test, you never really know,” said Joel Schwartz, an epidemiologist at Harvard University’s school of public health. “You might think you don’t have a problem, and you might be wrong.”
A NATIONWIDE PROBLEM
Reuters reviewed data from state health departments, the Centers for Medicare and Medicaid Services, and the CDC. Reporters sought testing information from health departments and Medicaid program administrators in each state, interviewed more than two dozen health experts, and spoke with 15 families whose children were poisoned.
Symptoms of under-testing span the country:
- Pennsylvania has childhood lead-poisoning rates nearly double Flint’s. But the state doesn’t require universal blood testing, so just 26 percent of children are tested by age three.
- At least three states – Utah, Kansas and Alaska – said they do not recognize or follow a federal requirement to test Medicaid children.
- Among the U.S. children for whom two tests are required by age three, millions receive no test or just one. Rates vary widely by state. Top performers test 80 percent of children repeatedly. South Carolina tested as little as 5 percent of Medicaid-enrolled children in 2014.
- After lead abatement efforts triggered a decades-long decline in child lead poisoning rates, the trend appears to be stalling. Based on testing results reported to the CDC, the percentage of children with blood lead levels double the agency’s threshold has remained steady, about 0.6 percent, the last five years.
The testing shortfall is one reason the CDC is unlikely to achieve its goal of eradicating lead poisoning among U.S. children by 2020, public health specialists say.
There are many causes for the gaps. Surveillance funding and data collection have been cut, and many states rely upon parental questionnaires to identify at-risk children to test. Several leave the testing option to pediatricians.
Testing guidelines, and the questionnaires, mostly target children in areas where older housing can expose them to lead paint. They often do not address another important risk, lead-tainted drinking water.
Ironically, the United States’ success in reducing lead poisoning is one reason for testing lapses. Lead was banned from most paints in 1978, from gasoline in the early 1980s, and, more recently, from new household pipes and fixtures. Average childhood lead levels have fallen by more than 90 percent since the late 1970s. Since then, however, research has shown that even low levels of exposure can stunt a child’s development.
Symptoms of poisoning – neurological impairment and behavior disorders – can be hard to distinguish at first. Once enough lead accumulates in blood and bone, the damage is irreversible. Negative health impacts of lead can begin at blood concentrations below the threshold used by the CDC, which says no level of exposure is safe.
LIFELONG STIGMA
Ingesting lead can sicken people of any age, but it takes the heaviest toll on small children, whose developing bodies readily absorb it.
By school age, children with a history of lead exposure can exhibit poor attention and impulse control, with lower intelligence and academic performance – a stigma that can follow them through life.
“The lower your IQ, the more trouble learning, the more likely you are to drop out of school, to be delinquent, to be incarcerated,” said Dr. Morri Markowitz, director of the lead poisoning program for the Children’s Hospital at Montefiore in New York City.
Although many exposure impacts are irreversible, poisoned children can benefit from therapy aimed at improving cognitive abilities. A high test result should be followed quickly by informing the family of lead risks, or intervention. Home inspections may spot sources of poisoning to be fixed.
As recently as the 1990s, the CDC recommended tests for all U.S. children. Since then, its guidelines have changed. The CDC still says all “at-risk” children should be tested but now encourages some states to devise a “targeted” approach.
After a 2012 budget cut, the CDC was forced to slash funding to states for lead poisoning prevention programs by some 90 percent. Though much of the funding was restored, several state health agencies cited dwindling CDC funding for their lead poisoning programs as one reason more children aren’t tested.
More than a dozen states do not report local testing results to the CDC. In many states using a targeted approach, parental questionnaires help decide which children to test, based on risk factors such as living in older housing.
Around 25 million older U.S. homes or apartments contain lead paint, with most located along the East Coast and in the Midwest.
Yet Flint serves as a potent reminder old paint isn’t the only exposure risk. Lead can leach into drinking water from pipes, a problem discovered recently in Mississippi, Ohio and at New Jersey and Oregon schools. Lead-tainted water from unregulated private wells is also a danger for up to six million Americans, Reuters reported in March.
Soil, cookware, and some imported toys, candies and spices can contain lead. Parents with careers or hobbies involving lead items – such as oil drilling, hunting or fishing – may bring the risks home.
Reuters reviewed the risk-assessment questionnaires health clinics give to parents in a dozen states. None asked about potential water contamination from lead piping or sink fixtures.
Before Flint, “lead risks were not being recognized as much, even though the research shows that there is no safe level of lead in blood,” said Dr. Jennifer Lowry, a pediatrician at Children’s Mercy Hospital in Kansas City. Chair of the Council on Environmental Health at the American Academy of Pediatrics, she supports universal testing.
A blood lead test is the only cheap and reliable way to identify a lead-poisoned child. Finger-prick testing at a pediatrician’s office can provide initial results in three minutes. The tests range in cost, from as little as $7.
ROOTS OF FAILURE
In Ohio, Joshua Sekerak wasn’t tested until he was two years old. He should have been tested a year earlier, because he was on Medicaid and lived in a high risk area.
Ohio mandates universal testing for children in ZIP codes where old housing is prevalent. About two-thirds of the state’s children should be tested under those rules. Ohio also requires tests for Medicaid children.
Actual testing falls short of Ohio’s guidelines, mirroring the U.S. problem.
Last year, Medicaid recorded payment claims for 41 percent of one- and two-year-olds enrolled in the insurance program in Ohio. The state’s Medicaid administration said some additional children were screened for free, but did not quantify how many.
Among all Ohio two-year-olds, less than a third got tested in 2014, state data show.
In Cleveland, a staggering 13.7 percent of children tested had lead levels above the CDC’s threshold, state data show. Following the contamination in Flint, 4.9 percent of children exceeded the threshold.
California, the nation’s most populous state, requires tests for all Medicaid children. Medicaid paid for enough lead tests to cover just one in three enrollees, last year’s claims data showed. “Improvements are needed” in testing and reporting, the state’s Department of Health Care Services told Reuters, vowing to redouble its efforts.
In some states, the testing gap is small. Vermont and Massachusetts screen around 80 percent of children repeatedly.
But across all 11 states that require universal screening, millions miss out.
“Only a fraction of the children who should be tested are being tested,” said Dr. Stanley Schaffer, who runs a pediatric program in industrial Rochester, New York.
New York State law requires testing for all children at age one and again at two. But statewide, only 55 percent of children have received their two required tests by age three, state data shows. Outside New York City, the rate drops to around 40 percent. In some counties, it’s below 10 percent.
Schaffer pushed measures to test as many children as possible, and the rate at his pediatric ward now reaches 90 percent.
Among the reasons for under-testing: Some doctors don’t order the tests or are unaware of the rules; children miss appointments or parents don’t follow up on test referrals; Medicaid and health departments do little to enforce testing requirements.
Medicaid has required testing of enrolled children since 1989, a CMS spokesman said. Arizona, the only exception, received a Medicaid waiver authorizing it to test only some enrolled children. To get it, Arizona showed it collects ample lead surveillance data to ensure at-risk children are referred for blood testing.
But health administrators in at least three other states told Reuters they do not require testing or recognize the federal mandate.
“There is no requirement in Kansas for Medicaid-enrolled children to be tested for blood lead levels,” said the state’s Department of Health and Environment.
Utah and Alaska also said they don’t require testing. In Utah, health official Sam Lefevre said the state has lower than national average lead poisoning rates, and its Medicaid children were not at higher risk.
That several states do not recognize the Medicaid requirement drew surprise from attorney Jane Perkins, a child healthcare advocate at the National Health Law Program.
In the 1990s, Perkins led a successful nationwide class action lawsuit to force laggard state Medicaid programs to comply with testing requirements. Now, Perkins says, her litigation team is investigating whether these states are flouting requirements.
AWAY FROM THE CAMERAS
Flint has become a symbol of mass failure to protect low-income children. When President Barack Obama visited May 4th, he urged all Flint parents to have their children’s blood tested for lead.
Less attention has been drawn to regions with higher lead poisoning rates.
A year after Flint’s switch to corrosive river water, nearly 5 percent of children tested there had blood lead levels above the CDC’s threshold. In as many as 11 states, the rates of poisoning surpass that mark, according to the agency’s data.
Across Pennsylvania, 9.4 percent of children tested in 2014 had levels above CDC’s threshold, a state report said. “There are probably a thousand kids in Philly with lead levels over 10 (micrograms per deciliter) and that number should be zero,” said Donna Cooper, executive director of the Philadelphia-based nonprofit Public Citizens for Children and Youth.
For at-risk children, testing should continue after age two, experts said.
In Ohio, after Joshua Sekerak was diagnosed with lead poisoning, weeks passed before a state inspector arrived at the family rental home. It was infested with lead paint, paint dust and contaminated soil.
Before Joshua’s diagnosis, his family was unaware of the lead exposure dangers, and their century-old rental house had passed a building inspection. With word of their child’s illness, the family moved to a new, lead-free home.
At age four, Joshua has the verbal skills of a child half his age. He uses diapers and drinks from a baby bottle. He needs therapy and psychiatric medications.
The special needs pre-school class Joshua attends recently sent the family a nylon harness device, to prevent injuries, and he is harnessed during the ride to school in the district’s van for children with disabilities. His attention span is around 15 seconds.
Shortly after Joshua’s lead poisoning was discovered, doctors told Serenak he also qualified for an autism diagnosis.
 Aaron Josefczyk/Reuters
Aaron Josefczyk/Reuters
At home one recent morning, Joshua showed a fascination with railroads. He lay down next to a toy track, repeating “choo-choo train.” He fixated on a tablet video of a freight train crushing a can on the rails, banged on doors and stared out the window.
When his dad came home from working on a farm, Joshua ran to him with a hug.
The house is several blocks from a busy freight train crossing. Jennifer Sekerak has installed alarms on the doors, but is haunted by the possibility Joshua may find a way out. “If that happens, he will go straight for the train tracks,” she said.
“I wish he’d been tested earlier,” the mother said. “I don’t know who to be angry with – the doctors, the landlord, myself?”
–
Previously:
* The Best Reporting (So Far) On The Flint Water Crisis.
* Item: Flint Hint.
* How Al-Jazeera America Reported The Flint Water Crisis – A Year Ago.
* A Flint Journal Reporter Explains How The Water Crisis Happened.
* Race Best Predicts Whether You Live Near Pollution.
* How The EPA Has Failed to Challenge Environmental Racism in Flint – and Beyond.
* We Helped Uncover A Public Health Crisis In Flint, But Learned There Are Costs To Doing Good Science.
–
Comments welcome.
Posted on June 9, 2016